Integrating Primary and Behavioral Healthcare: Key to Reducing Costs?
Bryan Robertson | June 24, 2016 | Care Providers, Chronic Conditions
When did we start differentiating “physical health” and “mental health?” Isn’t it all just health?
Treating patients holistically could be the secret to reducing healthcare costs while improving the quality of care. Sure, it might sound like an oxymoron – an impossible feat even – but is it?
Why Integrated Care?
All to often, this scenario takes place: a patient with a primary chronic condition, such as diabetes, visits a primary care doctor and is treated for that one chronic condition. But, of patients with chronic illnesses, an average of 43 percent have an additional co-occurring mental health condition, like depression, that often goes unrecognized and untreated.
The average cost of treating diabetes is $8,000 per patient per year. But, if that patient also has depression that isn’t discovered and treated, the cost for that patient’s care can jump to as much as $37,500 per year.
Several primary care doctors have said to me, "if I only could get my diabetic patients to behave". It's not a stretch to understand why a diabetic with a co-morbid major depressive disorder could be inconsistent in complying with her or his doctor's treatment plan. That inconsistency or non-compliance with the treatment plan can lead to increased expenses from emergency room visits to hospital readmissions along with additional diagnostic testing and possibly re-prescribing.
Diabetes is just one of these conditions with frequent co-occurring mental health conditions. The data shows most patients with chronic conditions have a higher rate of mental health issues as well and only a small percentage are being diagnosed and therefore treated for the co-occuring mental health issues.
One in five Americans has some form of a mental health issue and most are either going untreated or their condition is being overshadowed by another clinical issue. Integrating mental health into primary care might just be the key employers need to reduce healthcare costs.
Healthcare Expenditure: Employers
Healthcare spending isn’t just the government’s problem – all self-insured employers are trying to figure out how they can control costs without sacrificing the coverage they offer their employees. With healthcare costs increasing faster than inflation and eating into profits, employers are struggling to maintain a comprehensive benefits package that continues to attract top talent without eroding profit margins. But, when a patient is assessed and treated with complete patient health in mind, evidence suggests that recovery and costs incurred can dramatically improve – for the patient and employer.
Mental Health and Productivity
Poor mental health among employees is a major contributor to poor productivity in the workplace. High absenteeism, frequent disability and the need to hire temporary and part-time employees to supplement the workforce are costly expenses for employers. Maintaining a workforce, with healthy minds and bodies, can help significantly in reducing those costs and integrating behavioral health into care can help achieve that.
Conclusion
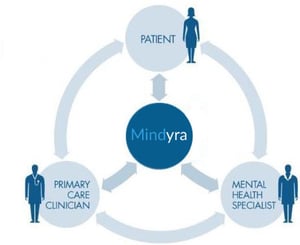
Behavioral conditions are complex and not easy to diagnose. Yet, they are such an important part of the patient’s overall health that screenings for them should be a normal occurrence, especially when the patient has a chronic physical condition. Family doctors should be given tools that encourage and empower them to test for all conditions, physical and mental, and treat them appropriately, because that’s what healthcare should be. It’s the whole patient – body and brain. And when employers integrate mental health they are not just saving money, they’re creating a more productive, happier and overall healthier workforce.

Join the Conversation